The Dawn of a New Era: India’s Groundbreaking Knee Surgery
Imagine a world where a debilitating knee injury, once a life sentence of pain and limited mobility, can be addressed with such precision that recovery feels almost… natural. Well, believe it or not, that world is becoming a reality, and India is right at the forefront of this incredible transformation. Just recently, a truly momentous leap forward occurred at Max Hospital in Delhi, spearheaded by Dr. Sujoy Bhattacharjee and his brilliant team at the Max Institute of Robotic Joint Replacement. This wasn’t just
any knee replacement, mind you. This was India’s very first robot-assisted cementless medial pivot knee replacement. Pretty big deal, right?
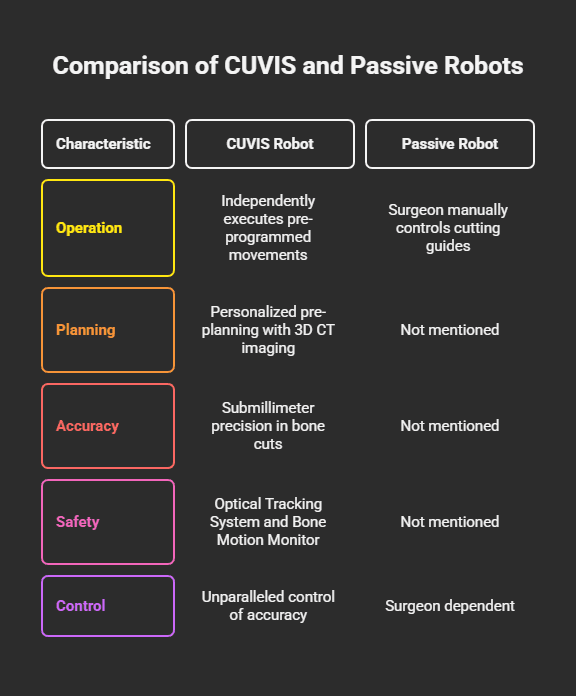
Initially, the doctors at Max were quite bold, claiming this was the “world’s first” such procedure. Now, that’s a statement that certainly grabs your attention, doesn’t it? But here’s the kicker, and it’s a crucial detail: the “world’s first” claim, while exciting, hinges on a very specific nuance. You see, while robot-assisted knee replacements aren’t entirely new, a similar procedure was performed in Louisville, Kentucky, in 2022 by Dr. Cyna Khalily using the CORI system; the distinction lies in the
type of robotic system employed. The CORI system, as Dr. Bhattacharjee clarified, was a passive robot, essentially guided and controlled manually by the surgeon. In stark contrast, the system used at Max, the CUVIS robot, is an
active robot. This means it’s capable of independently executing pre-programmed movements, which, according to Dr. Bhattacharjee, truly sets it apart as a global pioneer. This isn’t just medical jargon; it speaks to the level of machine involvement and the profound shift in surgical capability. It’s about pushing the boundaries of what the
robot itself can do, moving beyond mere guidance to a more autonomous, though still supervised, role.
So, why does all this matter right now? Well, the immediate impact is pretty profound: we’re talking about faster recovery, significantly reduced post-operative pain, and dramatically improved overall joint function. These aren’t just clinical terms; they translate directly into real-life improvements for patients, getting them back on their feet and living their lives with far less discomfort. The core of this innovation is a powerful trifecta of cutting-edge technology: precision robotics, a revolutionary cementless fixation method, and an anatomically designed implant. It’s a truly exciting time in orthopedic surgery.
Unpacking the “Cementless” Magic: A Closer Look at the Implant
Now, let’s dive into the fascinating world of cementless implants, because ditching the cement is, quite frankly, a game-changer. Traditionally, in knee replacements, the implant is fixed using bone cement, creating an artificial bond. But in this groundbreaking procedure, they opted for a cementless implant, primarily made of titanium. Think of it less like gluing something down and more like letting it grow roots.
The fundamental difference, and indeed the true magic, is how this works with the human body. The cementless approach allows the patient’s natural bone to grow into the implant, forming a biological bond. Dr. Ankush Sharma, a vital part of Dr. Bhattacharjee’s team, explained it beautifully: these implants are designed with microscopic pores, and the bone grows into these tiny spaces, locking the implant in place naturally. How cool is that? In contrast, traditional cemented implants rely on an artificial bond that, over a decade or two, can weaken and potentially lead to loosening. But with a cementless implant, once that biological bond is secured by bone growth, the chances of loosening are drastically reduced. It’s about building a foundation, not just a temporary fix.
Beyond just sticking around, the advantages of this cementless approach are quite compelling. For starters, there’s enhanced durability and stability because the natural bone ingrowth creates a much stronger, more integrated fixation. Then there’s the procedure itself: it’s quicker, eliminating the 12-15 minutes usually needed for the cement to set. In bilateral knee replacements, this alone can save nearly 25 minutes, and every minute counts in surgery, you know? Plus, there are reduced risks, including a lower chance of infection and a shorter hospital stay, all thanks to that biological bonding process. Who doesn’t want to get home faster? And here’s another big one: if, for some reason, a revision procedure is ever needed down the line, these implants preserve more bone stock, making future surgeries much easier. It’s like leaving options open. Oh, and it completely sidesteps complications like thermal necrosis, which can be caused by cement polymerization.
Now, every coin has two sides, and cementless implants do come with their own set of challenges and considerations. The biggest one? There’s absolutely no room for surgical error. Cement, in traditional procedures, can sometimes compensate for small inaccuracies, but with cementless implants, surgical expertise becomes even more crucial. It’s a high-stakes game, demanding the best. And, if I’m honest, the components themselves are generally more expensive. However, this can be offset by the savings from not using cement and the shorter surgical times. It’s a complex economic equation, for sure. Also, the proximal part of the tibia can be a bit of a weak link, prone to micromovements if not perfectly fixed. That’s why design matters so much, with features like taproots and lateral pegs added for optimal stability. Finally, it’s not a one-size-fits-all solution; this approach is best suited for patients under 65 with good bone quality where biological fixation is truly desirable.
The success of cementless implants, you see, is deeply intertwined with a quiet revolution happening in material science and manufacturing. It’s not just about “no cement”; it’s about what replaces it and how it interacts with the body. The evolution of materials directly impacts the success of these implants. For instance, early cementless designs faced issues, but today, we have incredible advancements. Materials like hydroxyapatite coatings are osteoconductive, meaning they actively encourage bone growth, even if there are tiny gaps. Then there’s porous tantalum, which offers optimal elasticity and a high surface coefficient of friction, allowing for a more physiological transfer of stresses to the bone around the implant. And let’s not forget 3D printing, which allows for the creation of highly porous titanium structures, like Tritanium, that mimic bone structure and enhance early stability and osseointegration. This represents a significant leap from earlier, less successful cementless designs. This highlights a broader, fascinating trend in orthopedic innovation: a relentless move towards biologically compatible and structurally optimized implants that truly work
with the body.
The Robot’s Touch: Precision, Power, and a Peek Behind the Curtain
Now, let’s talk about the robot itself, the CUVIS system, and how it’s transforming knee replacement from a highly skilled manual art into a precisely guided, technologically enhanced procedure. Think of CUVIS not as some sci-fi robot doing surgery on its own – no, no, not at all – but rather as the surgeon’s incredibly advanced co-pilot. It’s a high-tech tool that
assists surgeons, providing pinpoint accuracy that’s simply unmatched by traditional methods.
What truly sets CUVIS apart, and this is a key differentiator, is its “active” nature. Unlike “passive” robots, which are essentially cutting guides that the surgeon manually controls (like the CORI system used in that 2022 US surgery, remember? ), the CUVIS system is an active robot. It’s capable of independently executing pre-programmed movements. This isn’t just jargon; it describes a significant step towards greater robotic autonomy in surgery. While it still requires the surgeon’s oversight and the ability to halt the procedure if needed, its capacity for independent, pre-programmed execution moves well beyond mere guidance or physical manipulation. This trend towards more active systems promises even greater precision and reproducibility, potentially reducing surgeon fatigue and variability, though it certainly raises interesting questions about the evolving role of the human surgeon.
So, how does this robot work its magic with such precision? Well, it all starts with personalized pre-planning. Before a patient even enters the operating room, 3D CT imaging creates a detailed, three-dimensional view of their bones. This allows surgeons to craft a truly tailored surgical plan, ensuring that it’s
your knee, not a generic one, that’s being addressed. The system even offers adaptive options, allowing for multiple cutting possibilities and real-time modifications during the surgery itself. It’s like having a detailed blueprint that you can fine-tune on the fly.
When it comes to the actual procedure, CUVIS delivers unmatched accuracy. It ensures submillimeter precision in bone cuts, which is crucial for preserving healthy bone and protecting delicate soft tissue, ultimately minimizing complications. We’re talking about incredibly fine margins here, where every tiny bit of precision counts. And the milling cutter technology? It’s not just a fancy saw. This system reduces the force on delicate bones, lowering the risk of fractures and ensuring the smoothest possible implant placement. It’s about gentle, yet powerful, precision.
Safety, above all else, is paramount, and the robot has its own guardian angels, if you will. The Optical Tracking System (OTS) provides real-time data, constantly monitoring the “gap”, the space between the implant and the bone, at every angle of knee movement, whether the patient is sitting or standing. This is essentially the robot’s “eyes,” ensuring everything is perfectly aligned. And then there’s the Bone Motion Monitor (BMM), a critical safety feature. It detects even the tiniest patient movements during surgery and, get this,
halts the robot to prevent any errors. Imagine the peace of mind knowing that. For systems like CUVIS-Spine, and by extension CUVIS Joint, the core technology principles often overlap, meaning a force navigation system provides real-time feedback on applied forces, further enhancing precision and safety. It’s like having a sixth sense for pressure, making the surgery incredibly controlled.
Dr. Bhattacharjee himself, when speaking about robotic surgery, calls it “precise, evidence-based and fully trackable”. This speaks volumes about the data-driven nature of modern surgery. The overarching goal, he emphasizes, isn’t just to replace the knee, but to preserve key structures, especially ligaments like the posterior cruciate ligament, which plays a critical role in knee stability. It’s about restoring natural function, not just replacing parts, and the robot plays a pivotal role in achieving that delicate balance.
The CUVIS system truly exemplifies the evolving paradigm of human-robot collaboration in surgery. It’s not an autonomous robot operating independently, but rather an intelligent assistant that significantly enhances the surgeon’s capabilities, providing “unparalleled control of the accuracy of bone cuts, implant positioning, control of gap balance, and resultant hip–knee–ankle (HKA) axis”. This synergy allows for a level of precision and reproducibility that would be incredibly difficult, if not impossible, to achieve manually. Yet, it crucially retains the human element for complex decision-making and unforeseen circumstances. This collaborative model is a defining trend in the future of orthopedic surgery, demanding new skills and a different kind of expertise from surgeons.
Why Medial Pivot? Mimicking Nature’s Masterpiece
So, we’ve talked about the cementless magic and the robot’s touch. But what about the type of implant itself? This procedure utilizes a “medial pivot” knee design, and it’s gaining serious traction for a very compelling reason: its ability to replicate the knee’s natural, incredibly complex movement.
You see, the knee isn’t just a simple hinge that swings back and forth; it rolls and glides with a changing center of rotation throughout its arc of motion. It’s a marvel of biomechanical engineering. The medial pivot design is specifically intended to mimic these natural kinematics. It features a concave medial side and a less constrained lateral side, which creates a “ball-in-socket” type joint on the medial side, while allowing for more lateral translation. This design principle is based on the understanding that the knee is inherently stable medially and more mobile laterally. The goal? To reproduce that complex, natural motion, which is crucial for a knee that
Feels like your own.
The benefits of this “natural” feel are pretty significant. Studies have shown that medial-pivot knees provide greater stability than traditional designs. And stability, let’s be honest, is everything when you’re trying to move freely and confidently. It also allows for a more natural range of motion. But perhaps the most compelling benefit, and one that truly resonates with patients, is their preference for these implants. Patients often prefer medial-pivot knees by a three-to-one margin, reporting a “more natural feeling” of their prosthesis and minimal awareness of it during daily activities. This concept of a “forgotten joint score”, where a patient barely notices their artificial knee, is a huge measure of success. The design also aims to restore function by replicating natural motion and AP stability, addressing common issues like anterior knee pain and quadriceps avoidance that can plague traditional designs.
To make this even better, the medial pivot design is often combined with kinematic alignment. This technique aims to duplicate the patient’s pre-arthritic native joint line, effectively restoring ligament isometry and balance without the need for soft tissue releases. It’s about tailoring the surgery to
your unique anatomy, not just a generic template. The combination of medial-pivot implants with kinematic alignment leads to improved stability, a more natural range of motion, and ultimately, better functional outcomes, which, of course, translates into higher patient satisfaction. It’s a powerful duo, working in concert.
The emphasis on “forgotten joint scores” and patients feeling their knee is “more natural” reveals a significant evolution in orthopedic surgery. It’s a clear shift from merely relieving pain and restoring basic mobility to a profound focus on the
patient experience and their perceived normalcy. It’s simply not enough for the knee to just work; it needs to feel like its own, seamlessly integrating into their daily lives. This patient-centric approach is a powerful driver for innovation in implant design, like the medial pivot, and surgical techniques, such as kinematic alignment. It aims for a seamless integration of the prosthesis into the patient’s daily life, which is a more subjective but equally important measure of success in modern orthopedics.
Beyond the Buzzwords: Real Benefits for Real People
When you combine robot-assisted precision, the biological bond of cementless fixation, and the natural kinematics of a medial pivot design, the tangible improvements for patients are truly remarkable. It’s not just a collection of fancy medical terms; it’s about a quicker path to recovery, enhanced safety, and a promise of long-term stability.
Patients are experiencing significantly faster recovery times and reduced post-operative pain. Who doesn’t want that immediate relief? This also translates to shorter hospital stays , meaning patients can get back to their own beds and routines much sooner. The biological bonding process of the cementless implant further contributes to a faster and smoother recovery. Indeed, patients often return to function much more rapidly, which is incredibly motivating.
From a surgical perspective, there’s enhanced efficiency and safety. The procedure is quicker, especially for bilateral replacements, largely because there’s no cement setting time involved. There’s also a reduced risk of infection. And because these are often minimally invasive techniques, there’s less tissue damage , which, as you might guess, means less trauma and a quicker healing process. The robot’s precision ensures consistent and predictable results, significantly reducing the potential for human error.
Looking at the long term, the promise is even more compelling. Patients can expect improved overall joint function. That stronger, more natural integration of the implant with the bone leads to better long-term outcomes and drastically reduced chances of loosening. Ultimately, superior outcomes should lead to fewer revision surgeries down the line.
The true power of this procedure, it becomes clear, lies in the synergy between robotic precision, cementless fixation, and the medial pivot design. Robotic accuracy enables the demanding, error-intolerant cementless technique, while the cementless approach itself contributes to quicker surgery times and reduced infection risk. The medial pivot design, in turn, leverages this precision to achieve more natural kinematics and higher patient satisfaction. This isn’t just an additive effect; it’s a multiplicative one, where each advanced component makes the others more effective, pushing the boundaries of what’s achievable in patient outcomes. It’s quite remarkable.
The Patient’s Journey: Recovery, Satisfaction, and What the Studies Say
So, what does this all mean for the patient, in the real world? Well, the early wins are pretty clear: faster, less painful, and generally more satisfying.
In the short term, studies consistently show that robot-assisted Total Knee Arthroplasty (RATKA) leads to better outcomes in terms of pain, physical function, and overall patient satisfaction. Who doesn’t want that immediate relief after surgery? Several studies also demonstrate improved postoperative pain scores and a diminished need for inpatient opioid medications with RATKA. That’s a big deal for comfort during recovery. Patients have also experienced faster independent ambulation after RATKA, meaning they get on their feet sooner, which is hugely motivating. And, perhaps most importantly, a significant proportion of patients reported that the knee operated with RATKA felt less painful and more natural compared to a manually performed total knee arthroplasty (MTKA). This aligns perfectly with the goals of the medial pivot design. It’s no wonder, then, that the majority of patients who underwent RATKA would choose it again and recommend it to others. That’s a powerful endorsement, if you ask me.
However, when we take the long view, the picture becomes a little more nuanced, and this is where things get interesting. Some long-term studies, with follow-up periods averaging over ten years, suggest that robot-assisted TKA does not improve long-term clinical and radiologic outcomes when compared to conventional TKA. They found no statistically significant difference in overall clinical outcomes, the prevalence of outliers for hip-knee-ankle angle, or complications like revision surgery. More recent data, specifically looking at two-year follow-up for patients over 65, also found that robotic assistance in cementless TKA
does not improve revision rates. The odds of all-cause revision, or revision due to infection or mechanical loosening, were found to be similar between robotic-assisted and conventional groups.
So, why this apparent discrepancy? While single-surgeon studies often highlight improved precision with robotic assistance and potentially better early recovery or less soft tissue damage, larger registry studies, like the American Joint Replacement Registry, haven’t consistently shown the same long-term functional or clinical benefits. This could be due to various factors, including data limitations (for instance, 60% of entries in one registry didn’t even report if robotic assistance was used ), or simply that while precision is undeniably improved, it doesn’t always translate into
statistically significant long-term patient-reported outcomes or implant survivorship across large, diverse populations. It’s a complex puzzle.
What’s more, despite all these incredible advancements, it’s a sobering fact that up to 20% of patients still report dissatisfaction or ongoing knee pain after TKA. This underscores that even with cutting-edge technology, there’s always room for improvement, and individual patient variability plays a huge role.
The current research landscape presents a compelling narrative: while robotic assistance undeniably enhances surgical precision and provides tangible short-term benefits in terms of pain, recovery, and patient perception of a “natural” knee, its long-term impact on revision rates and overall clinical outcomes compared to conventional surgery is still a subject of ongoing debate and rigorous research. This suggests that while technological advancements like robotics are crucial for optimizing the
surgical act itself and improving the immediate post-operative experience, other factors, perhaps patient selection, adherence to rehabilitation protocols, or the inherent biological variability of bone healing and implant wear, might play a more dominant role in determining very long-term success and revision rates. It’s a powerful reminder that medicine is incredibly complex, and “better” in one aspect doesn’t automatically mean “better” in all. This also implies that future research needs to focus on identifying specific patient populations who might benefit most from RATKA and on continually refining long-term outcome measures.
To help visualize these findings, here’s a comparative look at outcomes:
| Outcome Metric | Robot-Assisted TKA | Conventional TKA | Source/Context |
| Short-Term Pain Scores | Improved, diminished opioid requirements | Higher pain, more opioid use | Short-term studies |
| Physical Function (Short-Term) | Better scores, faster independent ambulation | Lower scores, slower ambulation | Short-term studies |
| Patient Satisfaction (Short-Term) | Higher satisfaction, “more natural” feel, high recommendation rate | Lower satisfaction, less natural feel | Short-term studies, patient preference |
| Hospital Stay | Shorter | Longer | General trend |
| Implant Alignment Accuracy | Improved precision, lower outlier rates (tendency) | Higher outlier rates | Multiple studies |
| Long-Term Clinical Outcomes | No significant difference | No significant difference | Long-term studies (mean 129.1 months) |
| Long-Term Radiologic Outcomes | No significant difference | No significant difference | Long-term studies (mean 129.1 months) |
| Revision Rates (2-Year) | Similar odds of all-cause revision, infection, and mechanical loosening | Similar odds of all-cause revision, infection, mechanical loosening | Registry data (patients >65) |
| Overall Patient Dissatisfaction | Up to 20% still report dissatisfaction | Up to 20% still report dissatisfaction | General TKA statistics |
Navigating the Landscape: Cost, Accessibility, and India’s Unique Position
Let’s talk brass tacks: what does all this cutting-edge technology actually cost, and how accessible is it, especially in a vast and diverse country like India?
The price tag for a Robotic Total Knee Replacement Surgery (RTKR) in India can vary, generally ranging from ₹150,000 to ₹260,000, with an approximate average of ₹205,000. Now, that’s a significant sum for many, no doubt about it. But here’s where India truly shines on the global stage: this cost is considerably more affordable than in Western countries, where the same surgery could set you back anywhere from $30,000 to $50,000 or even more. This makes India a compelling value proposition for medical tourism, attracting patients from around the world.
However, a crucial detail for patients to understand is that many surgical packages do not include charges for high-end medical equipment like robots. Implants or prosthetics might also be extra unless specifically stated. So, it’s vital to ask all the right questions. While insurance is often accepted, patients absolutely need to consult their provider to fully understand their policy and any potential out-of-pocket expenses. Interestingly, some studies suggest that while the initial implant might be more expensive, the overall 90-day hospital cost for rTKA can be equivalent to manual TKA. This is due to factors like shorter tourniquet time during surgery and reduced complications. That’s a fascinating economic argument, hinting that the long-term value might offset the upfront cost.
Despite the relative affordability for international patients, India faces formidable accessibility hurdles internally. The country grapples with a poor orthopedic surgeon-patient ratio, roughly one surgeon for every 62,500 people, and these specialists are heavily concentrated in metropolitan areas. This leaves vast swathes of rural India, where 72% of the population resides, severely underserved. Beyond the human capital, there are significant infrastructure gaps. A scarcity of well-equipped hospital settings, a lack of proper patient referral systems, and suboptimal operating facilities in primary health centers often lead to delayed diagnoses and more complicated cases by the time patients finally reach a tertiary care center.
Furthermore, advanced technologies like robotics come with a steep learning curve and extensive training requirements for medical professionals. This isn’t something you pick up overnight; it demands significant investment in education and skill development. And, of course, the high economic burden of implementing and maintaining such high-tech systems is a substantial barrier, especially in resource-limited healthcare settings.
India, it seems, presents a fascinating paradox in the adoption of advanced orthopedic procedures like robot-assisted TKA. While the overall patient cost is significantly lower than in Western countries, positioning India as a global medical tourism destination, the
internal accessibility for its vast population remains a formidable challenge. The high initial investment in robotic systems, coupled with a concentrated surgeon workforce and an underdeveloped rural healthcare infrastructure, creates a two-tiered system. This implies that for such innovations to truly revolutionize healthcare across India, strategies must address not just the procedure’s cost but also the broader systemic issues of training, infrastructure development, and equitable distribution of advanced medical technology. The “cost-neutrality” argument is promising but needs to be evaluated within this complex national context.
What’s Next? The Future of Orthopedic Innovation
The field of orthopedics is undergoing a significant transformation, driven by incredible advances in technology and a deeper understanding of the human body. It’s an exciting time to be involved in this space, and robot-assisted surgery is just one, albeit crucial, part of this revolution. It offers undeniable benefits like improved accuracy, reduced complications, enhanced patient outcomes, and faster recovery times.
But what lies beyond robotics? The next frontiers are already here, and they’re pushing the boundaries of what’s possible.
Artificial Intelligence (AI)
It is increasingly being used for enhanced diagnosis and treatment planning. Imagine having a super-powered diagnostic tool that can analyze vast amounts of medical images and patient histories, identify complex patterns, predict patient outcomes, and even pinpoint high-risk individuals. AI can construct detailed 3D reconstructions, accurately localize fracture sites, predict optimal surgical approaches, and even generate personalized post-operative rehabilitation plans, all of which can drastically reduce preoperative preparation time and further enhance surgical precision.
Then there’s 3D Printing, which is revolutionizing the creation of customized implants and prosthetics. Imagine an implant made
just for you, tailored to your unique anatomy. Technology allows for incredible precision, improved fit and function, and ultimately, better patient outcomes.
Regenerative Medicine
It is another thrilling area. Researchers are exploring the potential for tissue repair and regeneration, such as cartilage restoration procedures or stem cell therapy, to address the root cause of pain and potentially delay or even eliminate the need for replacement surgery. This is about healing and restoring, not just replacing.
The continued focus on Minimally Invasive Procedures aims to further reduce muscle and tissue damage during surgery, leading to even faster recovery times and less pain. And the broader trend towards
Personalized Medicine means treatment plans are increasingly tailored to individual patient characteristics, ensuring the most effective care for each person.
Finally, Digital Health Technologies are changing how we monitor and follow up with patients. Remote monitoring using wearable devices and mobile apps can improve patient engagement and potentially reduce healthcare costs.
This convergence of multiple innovations like robotics, AI, 3D printing, and regenerative medicine is truly driving a shift towards comprehensive, truly personalized medicine. Diagnosis, planning, surgical execution, and post-operative care are all being optimized and tailored to the individual patient. This holistic approach promises not just improved surgical outcomes but also enhanced quality of life, reduced complications, and potentially even preventive care. It signals a move beyond simply “fixing” to actively “optimizing” and “regenerating.”
This exciting future also means the role of the orthopedic specialist is evolving. Surgeons will need to develop proficiency in these emerging technologies, understanding their applications and limitations, and seamlessly integrating them into their clinical practice. The future surgeon, it seems, will be as much a tech-savvy innovator as a skilled clinician.
Conclusions
The recent robot-assisted cementless medial pivot knee replacement in Delhi marks a significant milestone in India’s orthopedic landscape, showcasing the nation’s growing prowess in advanced medical procedures. This innovative approach, combining the precision of active robotic systems like CUVIS with the biological advantages of cementless implants and the natural kinematics of medial pivot designs, offers tangible short-term benefits for patients, including faster recovery, reduced pain, and a more natural-feeling knee. The emphasis on “forgotten joint scores” reflects a profound shift towards patient-centric outcomes, moving beyond mere functional restoration to a focus on perceived normalcy and quality of life.
However, while robotic assistance undeniably enhances surgical precision and provides immediate post-operative advantages, its long-term impact on overall clinical outcomes and revision rates, when compared to conventional surgery, remains a subject of ongoing research and nuanced debate. This suggests that while technology optimizes the surgical act and early recovery, other factors, such as patient biology and post-operative adherence, continue to play a critical role in very long-term success.
Furthermore, India presents a compelling paradox: offering these advanced procedures at a fraction of Western costs positions it as a global medical tourism hub. Yet, significant internal challenges persist, including a disproportionate surgeon-patient ratio, infrastructure gaps, and the high capital investment required for such technologies. For these innovations to truly transform healthcare across India, a concerted effort is needed to address these systemic barriers, ensuring equitable access and comprehensive training.
Looking ahead, the future of orthopedics is poised for even greater transformation, driven by the convergence of robotics with artificial intelligence, 3D printing for customized implants, regenerative medicine, and digital health technologies. This holistic, personalized approach promises to revolutionize diagnosis, treatment planning, surgical execution, and post-operative care, ultimately leading to more optimized, integrated, and individualized patient journeys. The orthopedic specialist of tomorrow will undoubtedly be a tech-savvy innovator, adept at leveraging these powerful tools to push the boundaries of patient care.