So. You’ve noticed more hair in the brush. You’re wondering what’s going on underneath. Normal. Losing hair can feel like a punch in the gut, an emotional wake‑up call. But hey, you’re not alone. There are over a hundred types of hair loss. Sounds scary, right? But the good news: most are diagnosable, even treatable. Let’s walk through how doctors figure out what’s happening with your hair.
First Things First: Medical History & A Friendly Chat
Doctors will start by asking about you. Not in a creepy way. (Well… maybe a little.) They want to know your story:
- When did this all start?
- Was it sudden or gradual?
- Any big triggers, stress, illness, new meds?
- Family history (think: male or female pattern baldness)?
- Other symptoms, like nail changes, itching, and flare‑ups?
This history is gold. It feeds right into diagnosing the different types of alopecia, each has its own little backstory.
Patterns & Symptoms: Eyes On the Scalp
Ok, now comes the physical exam. This is where things get interesting, and maybe a bit graphic. But don’t worry, I’ll explain it in plain English.
a. Types of Hair Loss Patterns
Patchy loss = alopecia areata?
Think round or oval bald spots, anywhere from the scalp to the eyebrows to the beard. Sometimes hair regrows in one spot even while another falls out. There might even be itching or a burning sensation before it appears.
Diffuse thinning hair = telogen effluvium?
All-over thinning, especially if you’ve had a shock to the system: major surgery, new meds, stress, or postpartum changes. Your hair follicles are going into the resting phase all at once.
Receding hairline or crown thinning = androgenetic alopecia
Also known as male/female pattern hair loss. In men, it’s that temple and crown combo; women usually see broad thinning across the top.
Traction alopecia
If you wear tight hairstyles, braids, buns, or scarves, you might notice thinning or baldness along your hairline.
Scarring alopecias (like lichen planopilaris, discoid lupus, folliculitis decalvans)…
These are less common but more serious, leading to permanent hair loss, often accompanied by itching, redness, pain, flaking, or pustules.
b. Other Clues: Nails & Hairs
- “Exclamation‑point hairs,” or those short broken hairs at the edges of bald patches? That usually points to alopecia areata.
- Nail pitting or ridges, don’t laugh, it’s a key dermatology clue often found in alopecia areata.
- Hair shaft damage or breakage, a sign of trichotillomania (hair‑pulling disorder) or styling damage.
The Pull Test & Magnifying Tech: Doctors Get Hands‑On
Hair Pull Test
The doctor gently grasps 40–60 hairs and pulls firmly. Normally, only a few hairs will come out. If many (four or more) are loose, something’s off, like telogen effluvium or active shedding.
Dermatoscope / Trichoscopy
This handheld magnifier lets doctors get up close to your scalp and hair follicles.
- With alopecia areata, you might see yellow dots, black dots, and broken hairs.
- Female pattern hair loss shows many miniaturized (thin) hairs clustered in one area.
- Scarring alopecias show inflammation, pustules, and clear destruction of follicles.
“Trichoscopy” is just the high‑falutin term for dermatoscopy; dermatologists do love their long words.
Extra Help: Blood Tests, Microscopy, Biopsy
Sometimes looking or pulling isn’t enough. Docs dig deeper:
- Blood tests: They might check your thyroid (TSH), iron levels, B12, vitamin D, hormones, or autoimmune markers, especially if they suspect telogen effluvium or lupus.
- Light microscopy of hair shafts: Helps identify structural damage (like trichorrhexis nodosa).
- Scalp biopsy: A small tissue sample used to diagnose scarring alopecias and nail down exactly what’s active. Usually, one biopsy is enough.
Yes, it might sound intense. But most of these are quick and low‑risk procedures.
Weave It All Together: Putting Clues Into Diagnosis
Here’s how doctors think, behind the scenes:
| Observation | Likely Diagnosis | Next Steps |
| Patchy bald spots + exclamation hairs + nail pitting | Alopecia areata (autoimmune) | Dermatoscope exam; maybe biopsy or blood tests |
| Diffuse shedding 2–3 months after a stressful event | Telogen effluvium | Pull test, blood tests to find the trigger |
| Physical exam often involves a psych evaluation, too | Androgenetic alopecia | Clinical exam, dermatoscope, check family history |
| Hairline thinning from tight styling | Traction alopecia | Ask about hairstyle practices, physical exam |
| Physical exam often involves a psych evaluation too | Scarring alopecia | Dermoscopy; scalp biopsy is essential |
| Broken, uneven hairs of varying lengths | Trichotillomania | Burning, redness, and scarring on the scalp |
Believe it or not, most of the time doctors can diagnose these types with just tools, tests, and a bit of pattern-spotting.
5. Why It Matters: Choosing the Right Treatment
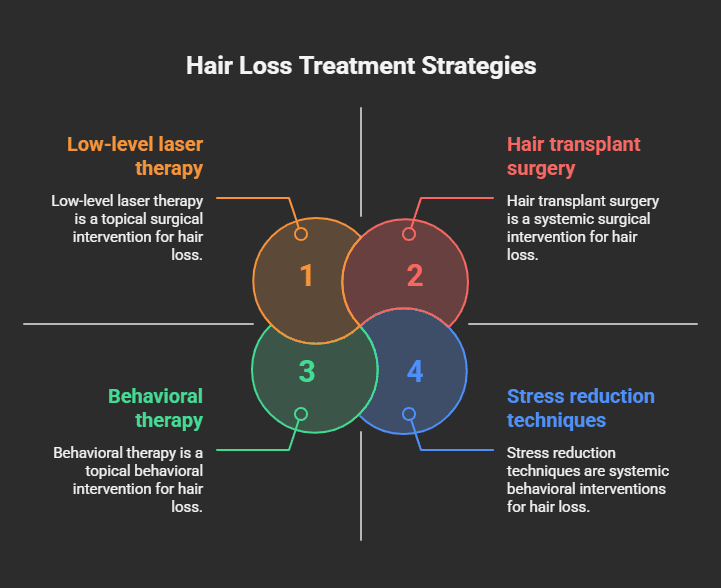
Here’s the kicker: each type of hair loss needs its game plan.
- Alopecia areata: often treated with steroids (topical or injections) or newer options like JAK inhibitors; sometimes hair just regrows on its own.
- Telogen effluvium: fix the underlying trigger, improve diet, adjust medications, and reduce stress. Hair often recovers in 3–6 months.
- Androgenetic alopecia: options include minoxidil, finasteride (for men), spironolactone (for women), low‑level laser therapy, or even hair transplant surgery.
- Traction alopecia: stop pulling on your hair. If caught early, regrowth is possible.
- Scarring alopecias: early diagnosis is critical; treatment involves anti‑inflammatories or immunosuppressants to prevent further loss.
- Trichotillomania: Behavioral therapy has shown better success than topical treatments.
Funny thing is, you could drop big money on generic hair remedies, but if you don’t know why your hair is falling out, those products are mostly snake oil.
When to See a Dermatologist vs. Just Your GP
Your general practitioner (GP) can handle most non‑scarring concerns, like pattern baldness, telogen effluvium, or early alopecia areata.
But you’ll want a dermatologist if:
- Scarring alopecia is suspected.
- You’re still unsure after the initial assessment.
- You’ve tried over-the-counter stuff with no improvement.
- It’s taking a real emotional toll; don’t beat around the bush; ask for help.
Dermatologists have access to advanced tools, dermatoscopy, scalp biopsy, and targeted blood panels, so they can give you a precise diagnosis.
Wrapping Up: What You Can Do Now
- Track your hair loss, note when it began, how it looks, and any triggering events. Even a simple journal helps.
- Book an appointment with your GP or dermatologist.
- Be prepared: a hair pull test might happen.
- Ask about tests like blood panels, biopsies, or dermatoscopy.
- Stick with the plan, once you have a clear diagnosis, treatments work so much better.
Final Thoughts: You’re Not Just Losing Hair. You’re Finding Answers.
Hair loss isn’t just cosmetic, it’s emotional, personal, and sometimes downright scary. But here’s the thing: knowledge is power. Once you know what’s happening, you can take real steps, doctor-led steps, that lead to real growth. Not just strands, but confidence.
Believe it or not, most hair loss can be diagnosed with a few simple tools: conversation, scalp examination, and maybe a gentle tug. And from there? Options. Treatments. Solutions that match your hair story.
So go ahead, share your story with a doctor. Get the full scoop. And if you want more tips on alopecia areata, telogen effluvium, pattern loss, scarring types, or just someone to rant to, I’m here for it.
You’ve got this.
Quick Recap (because life gets blurry)
- History & patterns = your starting clues
- Physical exam & specialist tools = identifying the type
- Tests reserved for complicated or scarring cases
- Treatment varies wildly depending on the diagnosis
- Early specialist input matters most for scarring forms
- Emotional support is key, hair is identity
P.S. Thought it’d all just be about minoxidil? Get it. But it turns out, it’s way more layered. Hang in there, and if you want me to explain JAK inhibitors, scalp biopsies, or emotional coping strategies next, just say the word.