In today’s busy and high-strung society, stress has become a nearly permanent fixture for many of us. But what if that persistent sense of being overwhelmed, that chronic stress, is doing more than merely making your daily life challenging? What if it’s quietly opening the door to an even more insidious challenge down the road – dementia? The link between stress and dementia is an increasingly relevant area of study and concern, and being aware of the relationship is the key to taking a preventive approach towards brain health. This article examines the intricate relationship between long-term stress and dementia in-depth, exploring the science, the risks, and, most importantly, what you can do.
It’s simple to write off stress as an unavoidable aspect of contemporary life. A difficult day at the office, money concerns, relationship tensions – all of these are usual stressors. It’s the chronic level of stress, the sort that persists day to day, that researchers are now recognizing as a major, but invisible, cause of cognitive impairment and, eventually, a higher risk of developing dementia. Though the stress-to-dementia process is lengthy and complicated, the evidence is strong enough to merit closer examination.
Getting to Know the Perpetrators: What Are Stress and Dementia, After All?
Before we untangle their relationship, let’s first appreciate these two terms independently.
What is Stress?
Stress, in its simplest terms, is the body’s automatic reaction to any stress or danger. When you feel threatened – be it a physical threat or a mental one, such as an impending deadline – your nervous system goes into overdrive, releasing a cascade of hormones, including adrenaline and cortisol. This “fight-or-flight” mechanism is meant to assist you in coping with the moment at hand.
- Acute Stress: This is temporary stress. It can be helpful, heightening your senses and giving you an energy boost when you need it most (e.g., slamming on brakes to prevent an accident). After the danger has passed, your body reverts to its normal state
- Chronic Stress: This is chronic, ongoing stress. It happens when the cause of stress is ongoing, or when the stress response is locked in the “on” mode. Typical causes are persistent financial struggles, unhappy work arrangements, extended caregiving, or lingering trauma. It’s this chronic type of stress and dementia that scientists are most interested in.
The body’s physiological reaction to long-term stress is having your body bathed in stress hormones all the time. This can result in:
- Increased heart rate and blood pressure
- Weakened immune system
- Gastrointestinal problems
- Sleep disturbances
- Mental illnesses such as anxiety and depression
- And, importantly, alterations in the brain.
What is Dementia?
Dementia is not a disease but a broad term for a variety of progressive neurological disorders that impair cognitive function. It’s a loss of memory, thinking, problem-solving, language, and judgment severe enough to interfere with daily life.
Common forms of Dementia:
- Alzheimer’s Disease: The most prevalent form, occurring in 60-80% of cases. It includes the formation of abnormal proteins (amyloid plaques and tau tangles) in the brain.
- Vascular Dementia: Frequently develops after a stroke or from conditions that injure brain blood vessels
- Lewy Body Dementia: Marked by unusual deposits of a protein called alpha-synuclein (Lewy bodies) in brain cells.
- Frontotemporal Dementia: Affects the frontal and temporal areas of the brain, causing personality, behavioral, and linguistic changes.
Symptoms of dementia are based on the type and location of the brain affected, but can be:
- Memory loss (particularly short-term)
- Trouble finding the right words
- Troubles with decision-making or judgment
- Getting lost in familiar environments
- Mood and behavior changes
- Trouble carrying out routine tasks
The Scientific Bridge: How Chronic Stress and Dementia Intersect
The notion that chronic mental stress might affect long-term brain health is not new, but new science is painting a more distinct picture of the mechanisms by which chronic stress and dementia are connected.
The Cortisol Connection:
When you’re under chronic stress, your body produces too much cortisol, commonly referred to as the “stress hormone.” Although cortisol is essential in limited amounts, chronically elevated levels can be harmful to the brain.
- Hippocampal Damage: The hippocampus is one area of the brain responsible for learning and memory creation – functions both severely compromised in dementia, and specifically in Alzheimer’s disease. Studies demonstrate that excessive exposure to elevated cortisol levels can harm and shrink the hippocampus. It can decrease neurogenesis (the growth of new neurons) and result in dendritic atrophy (shrinkage of the branches of neurons responsible for communication).
- Memory Impairment: Research has directly associated elevated cortisol levels with reduced performance on tests of cognitive function, including memory, executive function, and processing speed.
Inflammation: The Brain on Fire:
Chronic stress stimulates a low-grade inflammation within the body, including the brain (neuroinflammation).
- Dysregulation of the Immune System: Stress can interfere with the proper functioning of the immune system. In the brain, immune cells known as microglia may over-activate, releasing inflammatory chemicals that cause damage to neurons and their connections.
- Misfolding of Proteins: Chronic inflammation is considered to contribute to Alzheimer’s disease development by helping cause the misfolding and clumping of amyloid-beta and tau proteins – the disease hallmarks.
The HPA Axis Dysregulation:
The Hypothalamic-Pituitary-Adrenal (HPA) axis is the central stress response system of the body. Its dysregulation can be caused by chronic stress, or it does not shut off as it should.
- Prolonged Stress Response: Continuously active HPA axis implies the ongoing release of stress hormones, fueling the deleterious impact on the brain. This dysfunction is now more often regarded as a pivotal element on the road to chronic stress and dementia.
Effect on Brain Structure and Plasticity:
Outside the hippocampus, other important brain areas can be influenced by chronic stress:
- Prefrontal Cortex (PFC): It is responsible for higher-order cognitive processes such as decision-making, planning, and emotion regulation. Chronic stress can diminish PFC volume and disrupt its functions.
- Amygdala: The fear center of the brain. Hyperactivity and even enlargement of the amygdala can occur with chronic stress, and this can make people more sensitive to anxiety and stress, which are themselves risk factors for dementia.
- Decreased Brain Plasticity: Brain plasticity, or neuroplasticity, refers to the brain’s capacity to reshape itself through new neural connections. Chronic stress can undermine this adaptability and expose the brain to age-related changes and pathologies.
Indirect Pathways:
Chronic stress usually results in poor coping behaviors and lifestyle habits that are independent risk factors for dementia.
- Poor Sleep: Stress is a significant etiology of insomnia and disrupted sleep. Sleep is essential for brain detoxification (including amyloid protein removal) and memory consolidation.
- Unhealthy Diet: Stressed individuals are likely to consume comfort foods rich in sugar and unhealthy fats, which can lead to obesity, diabetes, and cardiovascular issues, all associated with an elevated risk for dementia.
- Deficient Physical Activity: Stress may drain motivation for exercise. Exercise is neuroprotective.
- Social Isolation: Withdrawal from social contacts can result from chronic stress. Social interaction is essential for cognitive well-being.
- Risk of Depression and Anxiety: These are highly associated with stress, and they are also considered major risk factors for developing dementia.
Chronic Stress and Dementia Risk: What Do the Studies Say?
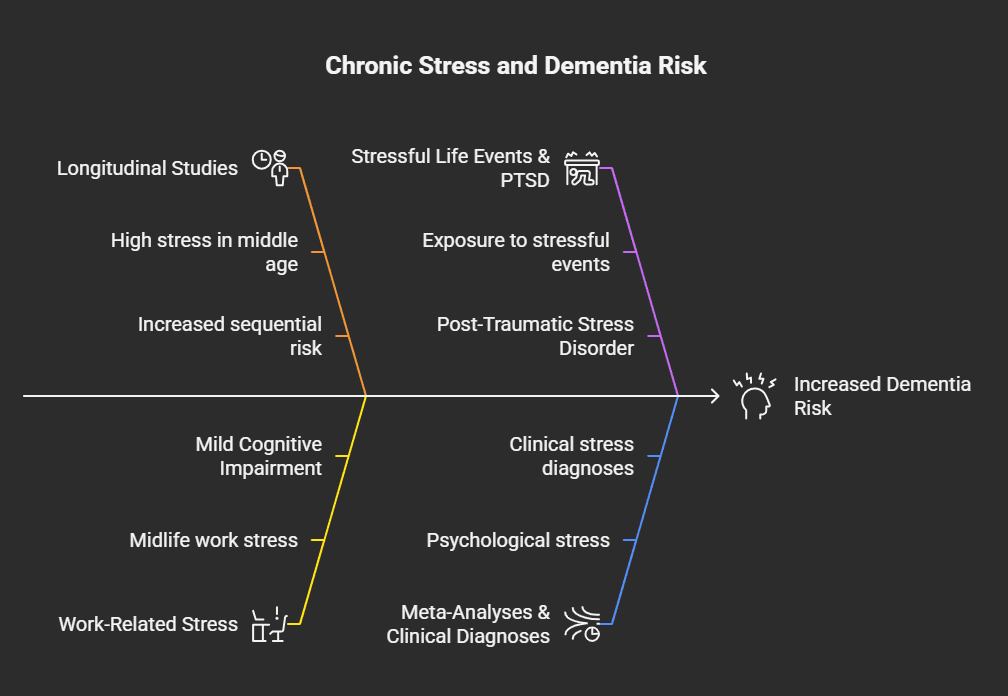
The link isn’t just theoretical; a growing body of research supports the connection between chronic stress and dementia:
- Longitudinal Studies: Longitudinal research on tracking people over decades has identified that individuals who reported high stress levels in middle age have a very high risk of developing dementia, including Alzheimer’s disease, in their old age. Increased sequential risk is indicated by some studies with more and longer experiences of stress.
- Work-Related Stress: Research focusing on midlife work-related stress has identified links with increased risk of Mild Cognitive Impairment (MCI – usually a harbinger of dementia), dementia, and Alzheimer’s disease.
- Stressful Life Events & PTSD: Having been exposed to a large quantity of stressful life events or having Post-Traumatic Stress Disorder (PTSD) has been correlated with a greater chance of cognitive decline and dementia.
- Meta-Analyses: Large-scale reviews combining data from multiple studies (meta-analyses) have consistently concluded that various forms of psychological stress, including perceived stress, neuroticism (a personality trait characterized by anxiety and negative emotions), and exposure to stressful life events, are associated with an elevated risk of both MCI and all-cause dementia.
- Clinical Stress Diagnoses: Those who are given clinical diagnoses of stress-related disorders during midlife also seem to have an increased subsequent rate of dementia.
It should be mentioned here that studies frequently wrestle with the inherently subjective nature of stress – what is enormously stressful to one is not stressful at all to another. But the replication across types of studies and measures of stress indicates a real and alarming relationship.
Can We Break the Cycle? Stress Management to Potentially Lower Dementia Risk
The silver lining is that even though chronic stress and dementia are associated with each other, dementia is not a foregone conclusion of a stressful life. Many of the contributors are reversible. By taking proactive steps to manage stress, we might be able to counteract its negative impact on the brain and possibly lower our risk for dementia. These evidence-based strategies are:
Welcome Physical Activity:
Routine exercise is a top stress-buster and brain booster.
- How it works: It slows down cortisol and adrenaline production, releases endorphins (natural mood elevators), increases blood flow to the brain, and fosters the growth of new neurons.
- Aim for: A minimum of 150 minutes of moderate-intensity aerobic exercise (such as brisk walking, biking, or swimming) weekly, plus muscle-strengthening exercises two times a week.
Prioritize Quality Sleep:
Sleep is when your brain washes itself and fixes memories.
- How it helps: Good sleep calms stress hormones and enables the brain to flush out metabolic waste, including Alzheimer s-related waste.
- Aim for: 7-9 hours of quality sleep each night. Establish a consistent sleep schedule, develop a calming bedtime routine, and turn your bedroom into a sleep sanctuary.
Practice Mindfulness and Meditation:
These methods can assist you in becoming more present in your thoughts and emotions without judgment, which decreases reactivity to stressors.
- How it helps: Ongoing practice can decrease cortisol, inflammation, increase attention, and even affect positive structural changes in the brain.
- Try: Mindfulness meditation, yoga, tai chi, or deep breathing exercises. Just a few minutes each day can have an impact.
Feed Your Brain a Healthy Diet:
Your diet has a direct effect on your brain health.
- How it helps: Anti-inflammatory foods high in antioxidants, omega-3 fatty acids, vitamins, and minerals may protect brain cells and oxidative damage.
- Emphasize: Diets such as the Mediterranean diet or the MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay), focusing on fruits, vegetables, whole grains, lean protein (primarily fish), nuts, seeds, and olive oil. Avoid processed foods, sweetened beverages, and excessive red meat.
Nurture Strong Social Ties:
Strong social connections and a busy social life shield against stress and mental deterioration.
- How it helps: Social engagement activates the brain, offers emotional support, and lowers loneliness and isolation, which are stress factors.
- Engage: Contribute to loved ones, participate in clubs, volunteer, or take courses.
Challenge Your Brain Continuously:
Stimulating your brain and keeping it occupied aids in the development of cognitive reserve – the brain’s resistance to damage.
- How it works: Acquiring new knowledge and participating in mentally challenging activities may enhance neural pathways and retard the development of cognitive symptoms.
- Activities: Puzzles, reading, studying a new language or instrument, playing strategic games, or acquiring a new hobby.
Reduce Unhealthy Coping Behaviors:
Reaching for alcohol, cigarettes, or too much caffeine to cope with stress can boomerang on your brain’s health.
- Why it works: Minimizing or removing these drugs decreases their direct adverse effect on brain cells and overall health.
- How to seek: Healthier means of stress management, like the above-mentioned techniques.
Identify Your Stressors and Learn to Manage Them:
Although you can’t always avoid stress, you can modify your reaction to it.
- How it assists: Knowing what triggers your stress enables you to create plans to avoid them or deal with your response to them better.
- Strategies: Prioritizing, boundary setting, problem-solving, cognitive restructuring, and learning to say “no.”
Take Professional Assistance When Necessary:
When stress becomes too much to handle or if you’re having any of the following symptoms: anxiety, depression, or ongoing memory issues, do not hesitate to seek help.
- How it assists: Therapists can offer coping mechanisms for stress, depression, and anxiety. Physicians can eliminate other conditions and offer proper interventions or referrals. Early evaluation of cognitive alterations is also very important.
When to be Worried: Identifying Early Warning Signs
It is normal to experience periodic memory slips or feel uptight from time to time. Nevertheless, the following signs may prompt a consultation with a healthcare provider:
Symptoms of Chronic Stress Overload:
- Recurrent feelings of worry, anxiety, or irritation
- Trouble concentrating or making decisions
- Ongoing feelings of being overwhelmed or drained
- Sleep changes (too much or too little)
- Changes in appetite or weight
- Increased alcohol or drug use to manage emotions
- Physical complaints such as headaches, muscle tension, or stomach problems
Early Warning Signs That Might Suggest Cognitive Decline (More Than Normal Aging):
- Forgetting recently acquired information, important dates, or recurrent feelings of worry, anxiety, or irritation
- Trouble concentrating or making decisions
- Ongoing feelings of being overwhelmed or drained
- Sleep changes (too much or too little)
- Changes in appetite or weight
- Increased alcohol or drug use to manage emotions
- Physical complaints such as headaches, muscle tension, or stomach problemsepeating the same questions over and over
- Problems with planning or problem-solving
- Difficulty with familiar tasks at home, work, or during leisure time
- Disorientation with time or place
- Difficulty with visual images and visual-spatial relationships
- New difficulty with words in conversation or writing
- Forgetting things and losing the ability to retrace steps
- Poor or decreased judgment
- Withdrawal from work or social life
- Mood and personality changes (e.g., becoming more easily confused, suspicious, depressed, fearful, or anxious)
If you or a family member is having a number of these symptoms, seeing a doctor is a good first step. Early detection of diseases such as MCI or dementia can result in improved management and care.
The Takeaway: Empowering Yourself Against Stress and Dementia
The link between chronic stress and dementia is a worrying issue, yet it is also a point of prevention. By learning how long-term stress can affect our brain’s health, we become empowered to take action. Stress management isn’t merely about living better today; it is an essential investment in your mental future.
While there are no promises in avoiding dementia, embracing a brain-healthy lifestyle that incorporates effective stress management can quite literally tip the scales in your direction. It’s making deliberate choices each and every day to nourish both your mind and body. The path to guarding your brain against the negative impacts of chronic stress and dementia starts with awareness and is maintained by regular, positive action.